By Andrea Hardy, Registered Dietitian, Canada.
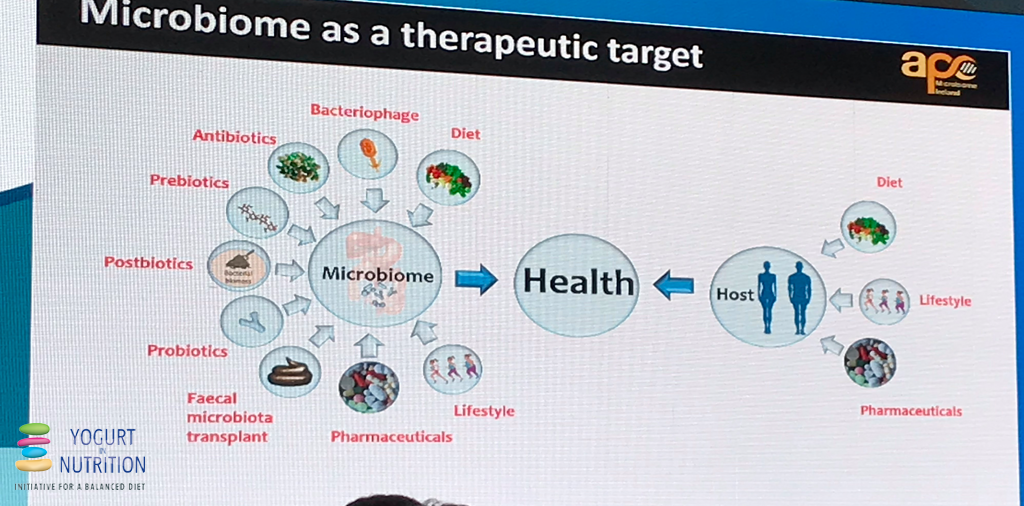
The science surrounding the gut microbiota is expanding. This year at the Gut Microbiota for World Health Summit, leading researchers explored how we can bring the science of the gut microbiome to health care.
It’s been believed that your gut microbiota begins to develop from the moment of birth, and plays a key role in training your immune system to function properly. New research by Kathy McCoy and colleagues have begun to uncover how the maternal microbiota influences development of an infant’s immune system, even before birth. This means that a healthy gut microbiota starts with mom, and likely starts preconception. Dr. John Cryan continued the journey of the microbiome through the lifecycle, exploring how the gut microbiota influences brain development through adolescence, highlighting the important role the gut microbiota plays in neural development and mental health. To round out the lifecycle, Dr. Paul O’Toole’s lab highlighted the role the gut microbiota plays in healthy aging, including frailty and cognition – emphasising that the health of our gut microbiota is something to consider through all stages of life.
How do we define a ‘healthy’ gut microbiota?
There is growing consensus that the microbiota is an ecosystem working together to keep us healthy, with no specifically defined structure. Researchers can agree that a greater variety and richness of bacteria is associated with better health outcomes, including reduced risk of chronic disease. Low richness (the number of species or genes in our microbiota) has been found to be common thread diseases like cardiovascular disease, autoimmune disease, neurodegenerative disease, and obesity.
How can we improve richness of our gut microbiota?
Dr. Colin Hill, this year’s keynote speaker said it perfectly: “You get the microbiota you deserve”. Meaning, there are many things that are in your control to improve the richness and diversity of your gut microbiota. This includes good nutrition, adequate sleep, stress management, exercise, and judicious use of medications.
“You get the microbiota you deserve” – Dr. Colin Hill, GMFH Summit 2020
Nutrition & Your Gut Microbiota
It appears that a variety of different nutrition interventions have benefits to our gut microbiota.
Hana Kahleova and her team have recently explored how a plant based, vegan diet positively influenced composition and function of the gut microbiota, inferring a health benefit to the participants. Participants were randomized to follow a plant based, vegan diet for 16 weeks, or to continue on their current standard American diet. After the 16-week intervention, those following the plant based, vegan diet were found to have a reduction in weight, and visceral fat, and an improvement in insulin sensitivity – all important markers in chronic disease prevention.
In Paul O’Toole’s lab, researchers explored how a Mediterranean diet influenced the gut microbiota and impacted healthy aging. These participants were randomized to receive a Mediterranean diet for 12 months, or to continue on their habitual diet. Those that received the Mediterranean diet experienced a positive change in the gut microbiota, reduction in inflammatory markers, improvement in cognitive function, and improvement in frailty scores.
How can you fuel your gut microbiota?
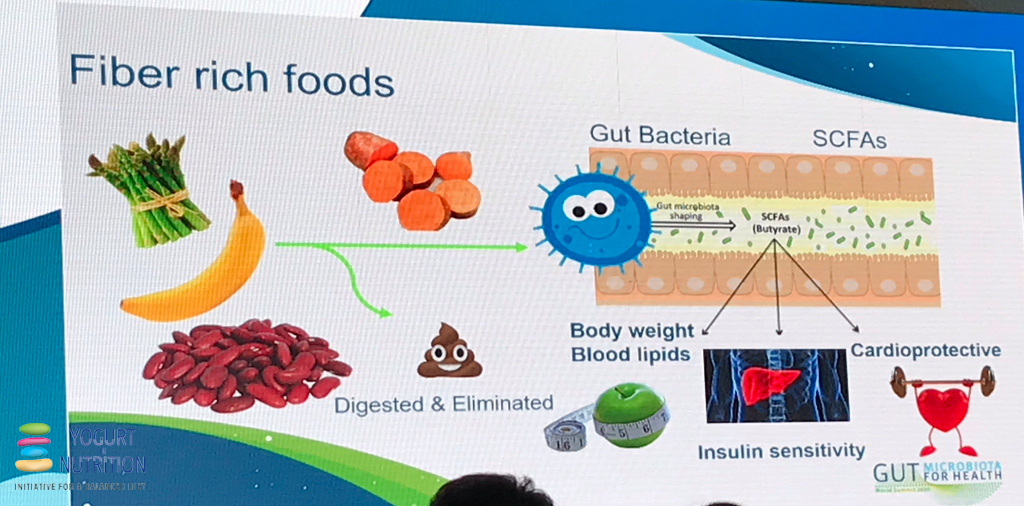
Hana Kahleova’s key message, regardless of what dietary pattern you follow is to “feed your gut microbiome well with whole plant-based foods.” This means including a variety of different foods with different types of fibre to encourage microbial richness. These dietary changes have been associated with improvement in gut microbiota profiles and functions – providing a measurable benefit to human health.
Some of my favorite tips are to:
- Enhance dietary variety by aiming for 30 different plant-based foods a week. This includes fruits, vegetables, whole grains, nuts & seeds
- Aim for 25-38 grams of fibre a day
- Include half a plate of vegetables at lunch and supper every day
- Choose a different whole grain at each meal – this could include oats, whole grain pasta, quinoa, sorghum, or buckwheat, for example
- Incorporate in 3 pieces or half cup servings of fruit a day
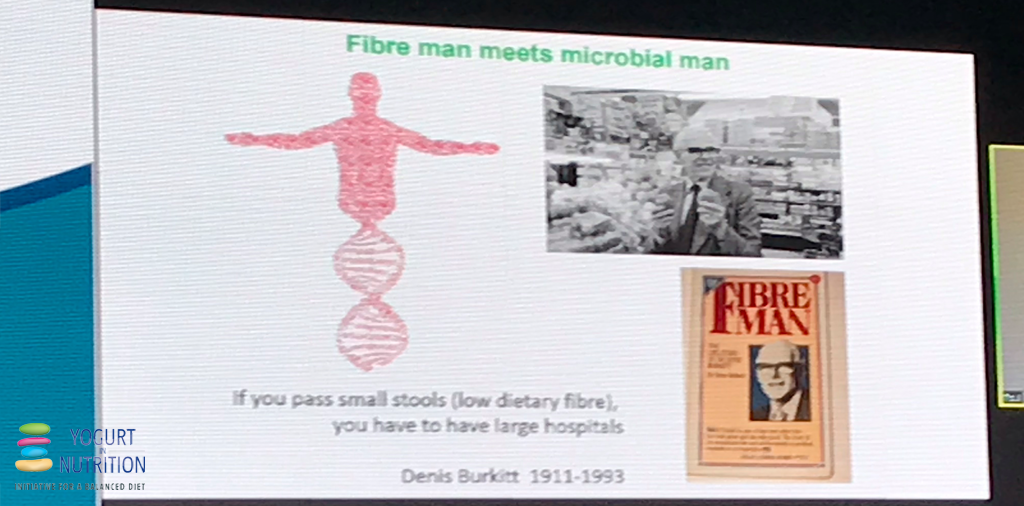
Each of these tips strive toward getting in a variety of fibre and what researchers have termed ‘macrobiota accessible carbohydrates’, or MAC’s for short. MAC’s are carbohydrates humans can’t digest, meaning they pass through the gut to the colon intact. In the colon, where the largest amount of our gut microbiota reside, they act as fuel for the bacteria. When bacteria are fed these important carbohydrates, they can thrive, and provide the body with important compounds, called short-chain fatty acids, which play an important role in immune function and inflammation.
Where do Fermented Foods and Probiotics Fit?
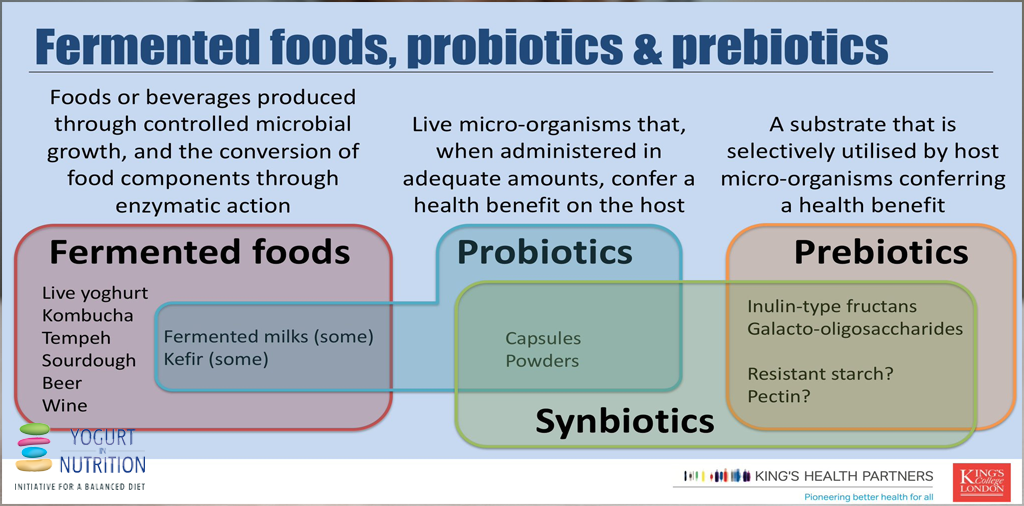
Dr. Kevin Whelan’s talk explored the differences between fermented foods and probiotics, and current evidence to support their uses, including the effects of yoghurt and cheese on human health which has been extensively reviewed elsewhere. Fermented foods are defined as “food or beverages produced through controlled microbial growth, and the conversion of food components through enzymatic reactions” and include foods like yogurt, kombucha, tempeh, beer, and wine. Not all fermented foods are probiotics, as probiotics have a very specific definition, being that they are “live organisms that, when administered in adequate amounts, infer a health benefit to the host“, and may be found in capsules, powders, or some yogurts & kefirs.
If you’re thinking “some yogurts” with added prebiotics are probiotics, it’s true. Some yogurts may meet the definition of probiotic (in the diagram “fermented milks”) but not all!
Currently, the research surrounding probiotics supports their proper use in only some conditions, like irritable bowel syndrome & ulcerative colitis – however, these effects are strain specific. To choose the right probiotic for the right reason, Dr. Whelan highlights the importance of working with your doctor, dietitian or pharmacist, as everyone does not need a probiotic for health.
At this time, there is only preliminary evidence on how fermented foods influence our gut microbiota – however there are still lots of great reasons to consume fermented foods! Fermentation can improve the digestibility of certain foods, such as dairy, by breaking down lactose. They also provide unique flavor and palatability, and offer a great way to introduce more variety to the diet.
Throughout all periods of life, there are crucial periods in which the gut microbiota plays a role. As Dr. Joel Dore emphasized – we must learn to live symbiotically with our gut microbiota – focusing on taking care of it, so it can take care of us. The key takeaway from the conference was that, as science evolves, there are important things we can do now to take care of your gut microbiota.
“A healthy, varied diet throughout the life span is your best bet to hedge possible gut microbiota benefits in all stages of life!”

 Registered Dietitian, Andrea Hardy from Calgary, Canada specializes in gastrointestinal disorders and the gut microbiome. She is recognized as Canada’s gut health dietitian – educating health care professionals and the public on the pivotal role nutrition plays in gut health. You can find her at Ignite Nutrition, or on Twitter (
Registered Dietitian, Andrea Hardy from Calgary, Canada specializes in gastrointestinal disorders and the gut microbiome. She is recognized as Canada’s gut health dietitian – educating health care professionals and the public on the pivotal role nutrition plays in gut health. You can find her at Ignite Nutrition, or on Twitter (